Human Rights
A human-rights-based approach to TB is grounded in international, regional and domestic law. These laws establish rights to health, nondiscrimination, privacy, freedom of movement, and enjoyment of the benefits of scientific progress, among others. Human rights law also establishes the legal obligations of governments and private actors. In order to implement a human-rights-based approach to TB, countries should:
- Prohibit discrimination against people with TB
- Empower people to know their TB status and
- Establish legal rights to access TB testing and treatment, including the elimination of financial and physical barriers to treatment and care
- Ensure the participation of people with TB in health policy decision-making processes
- Establish mechanisms to address rights of people with TB and ensure their implementation
- Protect the privacy of people with TB.
The Stop TB Partnership is working with all partners to ensure that all TB programmes are centered in a human rights based approach.
The Stop TB Partnership, in collaboration with KELIN and the International Human Rights Clinic at University of Chicago Law School, held a regional workshop on 24-25 June to promote the use of rights-based and community initiatives in TB work. The event, "TB, Human Rights and the Law", brought together 70 participants, including judges from countries in West, South, and East Africa as well as India and Australia; TB survivors; and legal, medical and public health experts to discuss the relationship between human rights, TB, and the law. . The workshop aimed to raise awareness of TB and the law and to sensitize judges in the region about the relationship between TB, human rights and the law.
The human rights-based approach to TB addresses inequities in treatment by emphasizing the rights of people living with and vulnerable to TB, including the rights to life, health, nondiscrimination, privacy, informed consent, housing, food and water. People affected by TB need to be able to claim their rights to information, participation, and informed consent; and win greater protections against discrimination through litigation and advocacy based on constitutionally derived human rights. There is a dearth of case law when it comes to TB as people have not exercised their right to protections against discrimination in employment, access to healthcare, and the armed services for example. In HIV there is explicit prohibition of discrimination based on HIV status through legislation in several countries but this is not the same for TB. If people are informed, they can use the rights approach to reduce stigmatization and increase their participation in policy decisions affecting their health.
This workshop in Nairobi built on the success of the "TB, Human Rights, and the Law" judicial workshop conducted in New Delhi, India on 19-20 December, 2015, and a KELIN, University of Chicago conference held in December 2014 entitled "Building a Rights-Based Approach to TB." Participants included members of the judiciary from East and Southern Africa, as well as people with TB, former TB patients, representatives from civil society and community groups, and legal, medical and public health experts.
The Tuberculosis, Human Rights and the Law Case Compendium was developed and written by the International Human Rights Clinic at the University of Chicago Law School as part of the TB and Human Rights Consortium, with support provided by the Global Drug-Resistant Initiative of the Stop TB Partnership.
The compendium is the first of its kind to present summaries of legal decisions involving TB from around the world. It contains more than 70 cases from 20 jurisdictions with translations of judgments in five languages, including from Brazil, China, India and other high burden countries. The compendium provides a global snapshot of the current state of TB case law, highlighting both the progress made in some areas and gaps in others. Cases are organized into 11 categories based on the issues involved. It was first used in the Southern African Litigation Center lawyers training March 13-16, 2017 in Johannesburg, South Africa.
Gender
A gender-based approach to TB aims at addressing the social, legal, cultural and biological issues that underpin gender inequality and contribute to poor health outcomes. It encourages activities that are gender-responsive investments to prevent new cases of TB, and strengthen the response to fulfil the right to health of women and girls, men and boys in all their diversity. Wherever applicable, these protections should be included in constitutional law or legislation. If this is not possible, they should be incorporated as legal rights in national and local TB policies.
The Stop TB Partnership and UNAIDS developed the first ever gender assessment tool for national HIV and TB responses to support counties in Global Fund applications which builds on the UNAIDS HIV Gender Assessment Tool launched in 2013 - and adapted to include TB. The tool assists countries to assess both the TB and HIV epidemics from a gender perspective. Findings from the assessment will help countries to make their responses gender sensitive and reduce the burden of TB and HIV. The HIV/TB Gender Assessment Tool seeks to move the HIV and TB response along the continuum from gender-blind to gender-sensitive, and ultimately to gender-transformative
(see Table 1). It makes use of a number of terms common to the HIV, TB and gender responses.
Gender Integration Spectrum
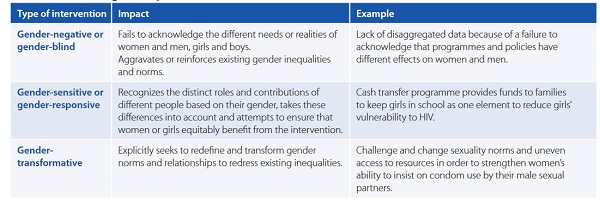
Source: UNDP 2014 http://www.undp.org/content/dam/undp/library/HIV-AIDS/HIV%20MDGs%20and%20Development%20Planning/UNDP-Checklist%20for%20Integrating%20Gender-May21-2014.pdf
Key Populations
This document is an action framework designed for implementers and countries to plan tuberculosis (TB) services for groups within their populations that are more vulnerable, underserved or at higher risk of infection and illness related to TB. These groups are referred to as key populations in the Stop TB Partnership Global Plan to END TB. They are key because addressing TB issues they face is critical to the overall goal of ending the epidemic for the entire population. Key populations vary by country and include people with increased exposure to TB due to where they live or work, people with limited access to quality TB services, and people at greater risk due to biological or behavioural factors. The document is a working draft and we look forward to your input to strengthen this work as you roll out the tools.
The powerpoint gives a brief overview of the document.
Global Plan to End TB and Key Populations
The Global Plan to End TB 2016-2020 outlines the following targets to be achieved by 2020 or 2025 at the latest.
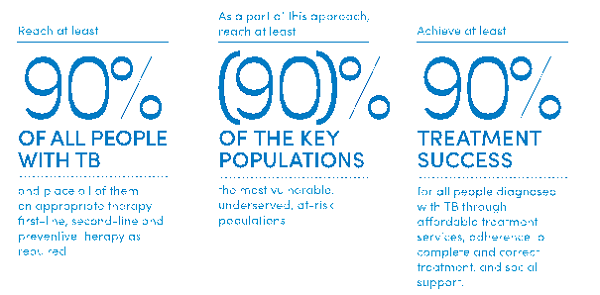
The Plan refers to people who are vulnerable, underserved, or at risk as TB "key populations" and provides models for investment packages that allow different countries to achieve the 90-(90)-90 targets. The Plan also suggests that all countries:
- Identify the key populations at national and subnational levels according to estimates of the risks faced, populations size, particular barriers to accessing TB care and gender related challenges.
- Set an operational target of reaching at least 90% of people in key populations through improved access to services, systematic screening where required and new case finding methods - and providing all people in need with effective and affordable treatment
- Report on progress in TB with data that are disaggregated by key population
- Ensure the active participation of key populations in the delivery of services and the provision of TB care in safe environments
In November 2015, the Stop TB Partnership hosted the first ever meeting of TB key populations in Bangkok, Thailand. The outcome of that meeting was the development of mini guides which define seven key populations that implementers need to consider when programming TB interventions. These populations (prisoners, miners, people who use drugs, PLHIV, healthcare workers, mobile populations, children < 5 years, rural and urban poor and indigenous peoples) all have specific needs in order to remove barriers to their accessing TB and TB/HIV services. These guides outline the key issues for each population and make recommendations on how we can remove barriers to access to prevention, diagnosis, treatment, care and support. Our aim is to now disseminate these guides and advocate for programs, implementers and donors to be responsive to the needs of key populations in TB.
The Partnership is now working to develop a framework to estimate the size and burden of TB in key populations. This framework will enable implementers to utilize tools we develop to address the specific need and demand for TB services in TB key populations. The framework and tool will be finalized in 2017 to enable their use in the next Global Fund allocation period.

