29 June 2015 - India -- *Meena visited the government hospital in the East Godavari district of Andhra Pradesh with cough and fever symptoms. Her sputum test revealed that she had TB. She was put on DOTS (anti-TB treatment). She was additionally counselled to get an HIV test done, which is a standard for TB care in India. Meena, however, chose not to get tested for HIV. When the TB health visitor made a home visit, he found that her HIV status was not known and she was once again advised to get the test done. She still did not comply. Under the TB-HIV Collaboration Framework, a line list of patients is shared. This list showed that Meena was recommended an HIV test, but had missed it. She was once again counselled and motivated to undergo the test. Finally, due to persistent efforts of healthcare providers, she got herself tested for the HIV virus. Her test results turned out to be HIV positive. She was immediately referred to the nearby Anti Retroviral Therapy (ART) center, along with treatment for TB. She was initiated on ART and after regular TB treatment for a duration of six months, she was completely cured of TB while she continued on ART.
In the absence of the TB-HIV Collaborative Framework currently well entrenched within the public health system in India, Meena would have received treatment only for TB, while her HIV would have been completely missed even though she had accessed health services. Additionally, her treatment outcome for TB may have been adverse.
Time is of essence and early diagnosis can be the difference between life and death. The good news is that Meena could access the integrated TB-HIV services. So, what has made this possible?
*name changed to protect patient’s privacy
Responding to a critical need
TB and HIV together form a deadly duo and can result in unfavourable outcomes for the patient, unless timely treatment is administered. This is because the HIV infection increases the risk of the progression of latent TB infection to active TB disease thus increasing the risk of death if not treated in time for both TB and HIV. TB is also the most common opportunistic infection and the main cause of mortality among people living with HIV (PLHIV). It is dif?cult to diagnose and treat owing to challenges related to co-morbidity, pill burden, co-toxicity and drug interactions.
The Global TB Report in 2014 highlights that India accounts for 2.6 million TB cases that make it 24% of the total global disease burden. About 40% of the population in India is estimated to be infected with the TB bacillus. Every year, 2.1 million people develop the disease and 240,000 die from TB annually. The adult HIV prevalence in India is 0.27%, which translates to 2.1 million people living with HIV/AIDS in India in 2011. HIV prevalence among incident TB patients is estimated to be 5.95%. About 120,000 HIV-associated TB patients are emerging annually in India. India accounts for about 10% of the global burden of HIV-associated TB. The mortality in this group is very high and among TB/HIV co-infected patients, 38,000 people die every year.
Adopting an integrated approach
TB/HIV collaborative activities between the Revised National Tuberculosis Control Programme (RNTCP) and the National AIDS Control Programme (NACP) started initially in the year 2001. Since then, TB/HIV activities have evolved in line with updated scientific evidences which have prevailed. The National Framework for Joint TB/HIV collaborative activities was developed under which the National and State TB/HIV coordinating mechanisms were put in place. Service delivery level coordination bodies were established at a district level. Components such as dedicated human resources, integration of surveillance, joint training, standard recording & reporting, joint monitoring and evaluation, and, operational research were strategically implemented and nationwide coverage was achieved in July 2012. At the national level, the TB/HIV coordination committee (NTCC) and technical working group (NTWG) regularly monitor and suggest on key policy related to TB/HIV Collaborative activities.
Progress so far
The interventions to reduce the burden of TB among people living with HIV include the early provision of antiretroviral therapy (ART) for people living with HIV in line with WHO guidelines and the three I’s for HIV/TB - i) intensified TB case finding followed by high quality anti-tuberculosis treatment, ii) isoniazid preventive therapy (IPT) and iii) infection control for TB. There have been significant improvements on the above indicators in the recent years.
The HIV testing of TB patients is now routine through provider initiated testing and counseling (PITC) implemented in all states. At the country level, as of the fourth quarter in 2014 (October-December), 74% TB patients knew their HIV status. This has increased from 11% in 2008. In 2014, 44,067 (5% of those tested) were diagnosed as HIV positive and were offered access to HIV care.
Similarly, among HIV-infected TB patients diagnosed in the fourth quarter of 2014, 93% were put on co-trimoxazole preventive therapy (CPT). The coverage of ART among TB patients who were known to be HIV-positive reached 91% in patients registered between October and December 2013 -- up from 49% in 2008.
Intensified TB case finding has been implemented nationwide at all HIV Integrated Counseling and Testing Centres (ICTCs) and ART centres. As of December 2014, 426 ART centres, and 927 link ART centres and 37 ART plus Centres are operating in the country. In 2014, 9% of total ICTC presumptive TB cases were referred to RNTCP and similarly, 3% PLHIV attending the ART centres were referred to RNTCP. With this, 4% additional TB cases were diagnosed at the national level.
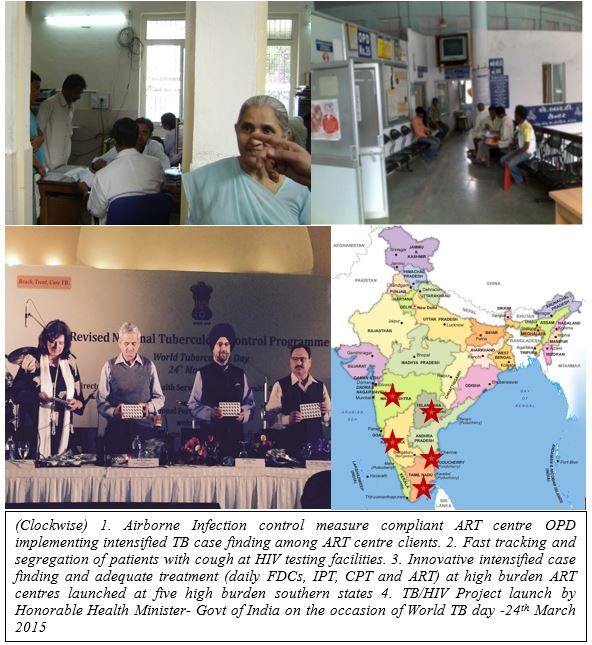
India has adopted all the recommendations suggested by WHO for TB/HIV collaborative activities. The Isoniazid Prevention Therapy (IPT) implementation plan has been approved by the NTWG which is now being implemented in a phase-wise manner. PITC among presumptive TB is being implemented in phase-wise manner in India. RNTCP has also endorsed the policy of prioritizing to offer rapid molecular test Xpert-MTB/Rif (CBNNAT) to all presumptive TB cases among PLHIV for early diagnosis of TB as well as Rif resistance. With support from WHO Country Office and USAID, RNTCP-NACP have joined hands for the implementation of ‘Innovative, Intensified TB case finding and appropriate treatment at selected 30 high burden ART centres in India’ aimed at reducing the burden of TB among PLHIV which was launched on World TB Day this year (24 March).
Key features of the project are
This synergy has proved to be extremely beneficial at multiple levels - for the patient, it means timely diagnosis and treatment with better health outcomes. For the health provider, it is an opportunity to ensure accurate and early diagnosis, and consequently correct treatment regimen. And, for the public health system, it means cutting down the chain of transmission, reducing the disease burden and saving lives. Much has been achieved in terms of putting in place systems and processes to ensure patients receive necessary care, but one cannot rest on one’s laurels. The words of the poet Robert Frost will serve as our inspiration - we have promises to keep and miles to go before we sleep.